eISSN: 2377-4304


Case Report Volume 6 Issue 1
Department of Obstetrics and Gynecology, Lilavati Hospital & Research Centre, India
Correspondence: Hemant Sunil Shintre, DGO, Post-diploma DNB resident, Department of Obstetrics and Gynecology, Lilavati Hospital & Research Centre, Mumbai- 400050, India, Tel 919967304921
Received: October 22, 2016 | Published: January 24, 2017
Citation: Shintre HS, Coelho KS. Managing Uterine Arteriovenous Malformation (AVM) is like dealing with raging wildfire awaiting a spark: better be extremely cautious & be ready with countermeasures like Uterine Artery Embolization (UAE). Obstet Gynecol Int J. 2017;6(1):23-26. DOI: 10.15406/ogij.2017.06.00195
Fewer than 100 cases of uterine arteriovenous malformation are reported which can cause life- threatening torrential hemorrhage. Prompt diagnosis and treatment are necessary with keeping differential diagnosis of retained products of conception and gestational trophoblastic disease in mind in cases of post-pregnancy or post-abortal arteriovenous malformation. We report a case of 27 year old young nullipara female who presented with post- abortal bleeding caused by uterine arteriovenous malformation and retained products of conception. Doppler and MRI results were inconclusive about exact nature of lesion. With uterine artery embolization facilities kept ready, evacuation of retained products was carried with utmost care under ultrasonography guidance. Still it caused torrential life-threatening bleeding which was successfully tackled by uterine artery embolization with an added advantage of preserving her future fertility.
Keywords: Uterine arteriovenous malformation, Color doppler, Angiography, Uterine artery embolization, Gestational trophoblastic disease
AVM, Arteriovenous Malformation; UAE, Uterine Artery Embolization; β-hCG, β-Human Chorionic Gonadotropin; USG, Ultrasound; MRI, Magnetic Resonance Imaging; DSA, Digital Subtraction Angiography; hPL, Human Placental Lactogen
Uterine arteriovenous malformation (AVM) is a relatively rare but potentially life-threatening condition.1 The true incidence of uterine AVM is not known. To date, only case reports or small case series exist, making it impossible to estimate true incidence. Fewer than 100 cases are reported in literature.2-4 Vascular lesions of the uterus are now thought more common than thought previously because of availability of better imaging modalities, more cases are being reported.5 It may result in profuse or irregular bleeding from abnormal connections between arteries and vein. It is seen as heavy abrupt vaginal bleeding, which may be postpartum, post-abortion, or menstrual and which is refractory to conventional therapies & life- threatening.6 Uterine AVM may be congenital or acquired. Congenital AVMs have multiple vascular connections, may manifest at other sites, and involve surrounding structures, whereas acquired AVMs usually have a single connection between an artery and a vein. Acquired AVMs may be preceded by uterine curettage, cesarean section, gestational trophoblastic neoplasia, or endometrial carcinoma. Pregnancy is thought to play a role in their pathogenesis. Chorionic villi necrosis followed by incorporation of venous sinuses in scarred myometrial areas may lead to formation of an AVM. AVMs are hormone responsive and congenital AVM may manifest at puberty or after a pregnancy.5
Prompt diagnosis and treatment are necessary. AVMs are diagnosed by Color doppler, ultrasonography, computed tomography, magnetic resonance imaging & angiography. Color doppler is a useful non-invasive method of initially diagnosing, confirming by characteristic mosaic pattern, high velocity high turbulent diastolic arterial flow within AVM and following up for resolution after treatment.7 Management depends on hemodynamic stability and the amount of bleeding as well as on the patient’s age and her desire to preserve fertility. Conservative management is the preferred method of treatment in order to avoid a hysterectomy in patients of child-bearing age. Selective uterine artery embolization is currently considered the treatment of choice in women of all age groups.5
A 27 years old woman who was a known case of Thalassemia minor was referred to our hospital. She presented with heavy bleeding per vaginum with passage of clots since two days. Patient gave history of continuous on & off minimal to moderate bleeding per vaginally after second trimester therapeutic abortion which was done two months back. Therapeutic abortion was done as chorionic villous sampling showed fetus being Thalassemia major (both husband & wife - Thalassemia minor). The therapeutic abortion was induced with the help of misoprostol (PGE1) tablets. According to the obstetrician’s notes conducting the therapeutic abortion, the abortion was complete and hence no curettage was done following the abortion. Patient had undergone another therapeutic abortion 8 months back for the same reason i.e. chorionic villous sampling indicating Thalassemia major fetus. This therapeutic abortion was followed by curettage of uterine cavity for complete evacuation of products of conception. Patient had no history of any other significant medical illness or surgical intervention in past.
On examination, the patient was afebrile, pale but hemodynamically stable. All the systemic examinations were within normal limits except on per speculum examination, partially open cervical os was seen with minimal clots. Patient had no active bleeding. On per vaginal examination, the uterus was bulky (8-10 wks size), firm to soft in consistency, mobile and with the free fornices.
Complete investigation work-up including complete blood count (Hb-9.5g/dL, platelets-3 lakhs), serum β-human chorionic gonadotropin (β-hCG- 35mIU/ml), normal coagulation profile & liver function tests were carried out. Blood sample was sent for cross matching and blood was kept reserved & ready.
Imaging studies like ultrasound & MRI- pelvis with contrast were done. MRI (Figure 1) was s/o bulky uterus with 4×7×7 cm sized heterogeneous lesion seen in posterior wall, lost endometrial-myometrial interface, multiple dilated tortuous blood vessels in posterior myometrium suggesting possibility of retained products of conception or gestational trophoblastic neoplasia (possibility of Placental Site Trophoblastic Tumor) or uterine vascular malformation. Transabdominal USG of the pelvis (Figure 2) revealed 8.8 cm× 7.5 cm× 7.5 cm bulky uterus the posterior myometrium markedly enlarged and heterogeneous with increased vascularity on Doppler. Doppler showed a peak systolic velocity (PSV) of 121 cm/s and resistive index (RI) of 0.36 i.e. high velocity, low resistance flow. USG also showed that endometrium was thickened (ET-14mm) in the lower uterine segment suggestive of retained products of conception.
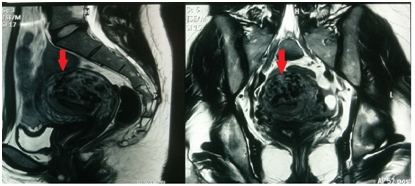
Figure 1 MRI pelvis- sagittal and transverse section- showing bulky uterus with 4x7x7 cm sized heterogenous lesion seen in posterior wall, lost endometrial- myometrial intergace, multiple dilated tortuous blood vessels in posterior myometrium & tiny enhancing area within the endometrium in lower uterine segment.
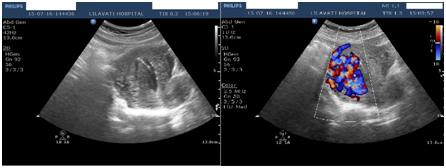
Figure 2 USG-pelvis revealed 8.8cm x 7.5cm x 7.5cm bulky uterus the posterior myometrium markedly enlarged and heterogeneous with increased vascularity on Doppler. Doppler showed PSV of 121cm/s & RI of 0.36 i.e. high velocity, low resistance flow. ET-14mm in lower uterine segment.
Chest X-ray revealed normal findings. Patient was posted for USG guided evacuation of retained products of conception with uterine artery embolization facility kept ready. Under general anesthesia under real time-USG guidance with the help of ovum forceps the retained products of conception from lower uterine segment evacuated with extreme care & sent for histopathology. In spite of extreme care taken, the evacuation triggered active bleeding. Immediately patient was taken for angiographic uterine artery embolization. The uterine artery embolization was done with the help of cyanoacrylate (glue) (Figure 3). No active bleeding was seen post-embolization. The patient was given good prophylactic antibiotics post-embolization. The patient was discharged on day-3 post-op on oral antibiotics & haematinics.
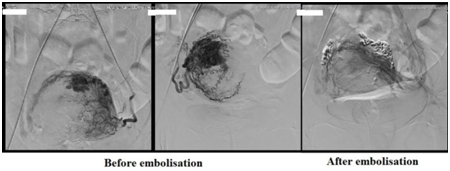
Figure 3 Digital substraction angiography (DSA) showing bilateral hypertrophy of uterine arteries that feed a tortuous, hypertrophic arterial mass with capillary lakes and post uterine AVM embolisation film demonstrating successful embolisation of the feeding vessels of AVM with the help of N-butyl cyanoacrylate(glue).
Histopathology of the tissue revealed degenerated and necrosed bits of decidua and few degenerate chorionic villi admixed with fibrin and blood s/o retained and degenerate products of conception (No features of Placental site trophoblastic tumor). After 6 weeks, patient was followed up & it was found out that per vaginal bleeding had diminished gradually over the period of 4 weeks & stopped completely thereafter. The pelvic ultrasound with Color Doppler confirmed diminished size of AVM with diminished vascularity (Figure 4).
Arteriovenous malformations (AVMs) can occur in any organ in the body, including the pelvic vasculature and rarely in the uterus. The first case of AVM was reported in 1926.8 AVM consists of proliferation of arterial and venous channels with fistula formation and a mixture of capillary-like vessels. Uterine AVM may be congenital or acquired. In our case, there was past history of post-abortal uterine curettage suggesting possibility of acquired AVM. The precise diagnosis of AVM is of vital importance. Traditionally diagnosis was made after hysterectomy & histopathological examination. Digital subtraction angiography remains the gold standard of diagnosis. However, it is rarely performed for diagnosis alone due to its invasive nature and is usually reserved when a patient requires surgical intervention or embolization.
Gray scale ultrasound can detect the presence of multiple tubular or ‘spongy’ anechoic or hyperechoic areas within the myometrium of a normal endometrium. However with the availability of non-invasive Color Doppler, it has become important modality for obtaining more accurate diagnosis. A normal myometrial signal will show a PSV of 9-44 cm/s and RI of 0.6-0.8. The spectral flow Doppler reveals the systolic and diastolic velocities 4 to 6 times higher than observed in normal myometrial vessels. Classically, the Color Doppler demonstrates the vessel structure with multidirectional high-velocity flow that produces a “color mosaic pattern,” and the spectral Doppler analysis typically shows high-velocity flow with a low resistance index that indicates arteriovenous shunting.3
The retained products of conception may also give a hypervascular appearance with turbulent flow. There are reported cases in which residual placental tissue complicated the diagnosis of uterine vascular malformation.9 Care needs to be taken before diagnosing AVMs during pregnancy and after abortion. All patients showing a hypervascular lesion in the myometrium must undergo work-up for retained product of the conception.5
Gestational trophoblastic disease may also have similar increased vascularity with a low RI.10 Elevated hCG levels are seen in this condition. However, a rare form called placental site trophoblastic tumor does not produce high levels of hCG, and instead produces high levels of human placental lactogen (hPL).
In our case, Doppler USG & MRI findings were characteristically favoring the diagnosis of uterine AVM with retained products of conception with possibility of GTD. The low β-hCG levels, normal chest X-ray suggested low possibility of gestational trophoblastic disease. Traditionally, hysterectomy or uterine artery ligation was the treatment for uterine AVM. Actually management depends on hemodynamic stability, the amount of bleeding, the patient’s age and her desire to preserve fertility. Acute treatment involves stabilizing the patient’s hemodynamic status, and stopping blood loss.
Currently, angiographic uterine embolization is the preferred treatment because it is minimally invasive and has a potential to preserve fertility.3,5,6 Some authors mention about placental abnormalities in subsequent pregnancies after UAE while some authors report normal pregnancies after UAE.3 Currently, there is no strong evidence about TAE induced persistent ovarian failure, major complications of pregnancy, or fetal growth restriction.3,11 Various embolic materials like polyvinyl alcohol, cystoacryl (glue), coils, balloons, haemostatic gelatin have been used. Cystoacryl (glue) is superior in cases where multiple small and large feeding vessels are present in AVM being liquid and slow-absorbable. Some cases may require repeat embolization.
Intrauterine balloon tamponade therapy has been described in literature in case of bleeding from non-pregnant uterus too. Some authors report successful management of bleeding in case of uterine arteriovenous malformation by use of only intrauterine balloon tamponade.12 While some report use of it as initial measure to tide over the critical period till definitive management either in form of embolization therapy or hysterectomy is made available.13,14 Bakri balloon or Foley’s catheter can be used for purpose of intrauterine balloon tamponade. There is no definite evidence that exclusive use of intrauterine balloon tamponade to arrest bleeding in case of uterine arteriovenous malformation is effective. So, combining it with other measures to ensure efficacy, using it as one of the first-aid measure to buy time for transfer in case of low-resource settings or using it to stabilize patient till arrangements for definite therapies like embolization or hysterectomy are made, is justified.
In cases of single episode of bleeding or hemodynamically stable patients who have the ability for close follow-up, expectant and long term medical management can be tried. The medical management includes estrogens and progestins, methylergonovine, danazol, 15-methyl-prostaglandin F2-alpha, oral contraceptives & intramuscular followed by oral methylergonovine maleate.15 Gonadotropin-releasing hormone agonists have been used as an adjunct to embolization to reduce the size of uterine AVM.16. This therapy may be useful in situations where embolization needs to be postponed.
Other surgical managements reported less frequently are coagulation of AVM under hysteroscopy guidance, surgical removal of AVM, laparoscopic bipolar coagulation of uterine vessels, and ligation of uterine vessels. Currently, hysterectomy is only reserved for women who do not need fertility preservation, in case of emergency in resource-poor settings where embolization facilities are not available, or in whom embolization therapy fails.1,5
The present case is interesting and underlines the importance of precise diagnosis, utmost caution, availability of medical facilities and correct application in successful management of uterine AVM. The case also indicates that angiographic embolization of AVM is a promising intervention in cases where fertility preservation is needed. Successful results have been reported after short period of time (6 weeks), but long term follow-up will determine the true success rate of these procedures.
Uterine arteriovenous malformations, either congenital or acquired, are very rare. They can lead to torrential life-threatening hemorrhage. Therefore, extreme care needs to be taken before diagnosing and managing AVMs during pregnancy and after abortion keeping the differential diagnosis of retained products of conception and gestational trophoblastic disease in mind. Angiographic Uterine Artery Embolization is the preferred therapy for uterine AVMs, especially in young women who desire to preserve fertility. However more research is needed to throw light on etiopathogenesis of uterine arteriovenous malformations and long term safety profile of uterine artery embolization in case of uterine arteriovenous malformations.
None.
None.

©2017 Shintre, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.